
“We are what we repeatedly do. Excellence, then, is not an act, but a habit.”
Misattributed to Aristotle as this quotation may be, the idea that consistency is critical for success is loudly affirmed by among others the world’s top athletes, business tycoons, and Dr Kristaps Jurjāns of Pauls Stradins Clinical University Hospital in Riga, Latvia.
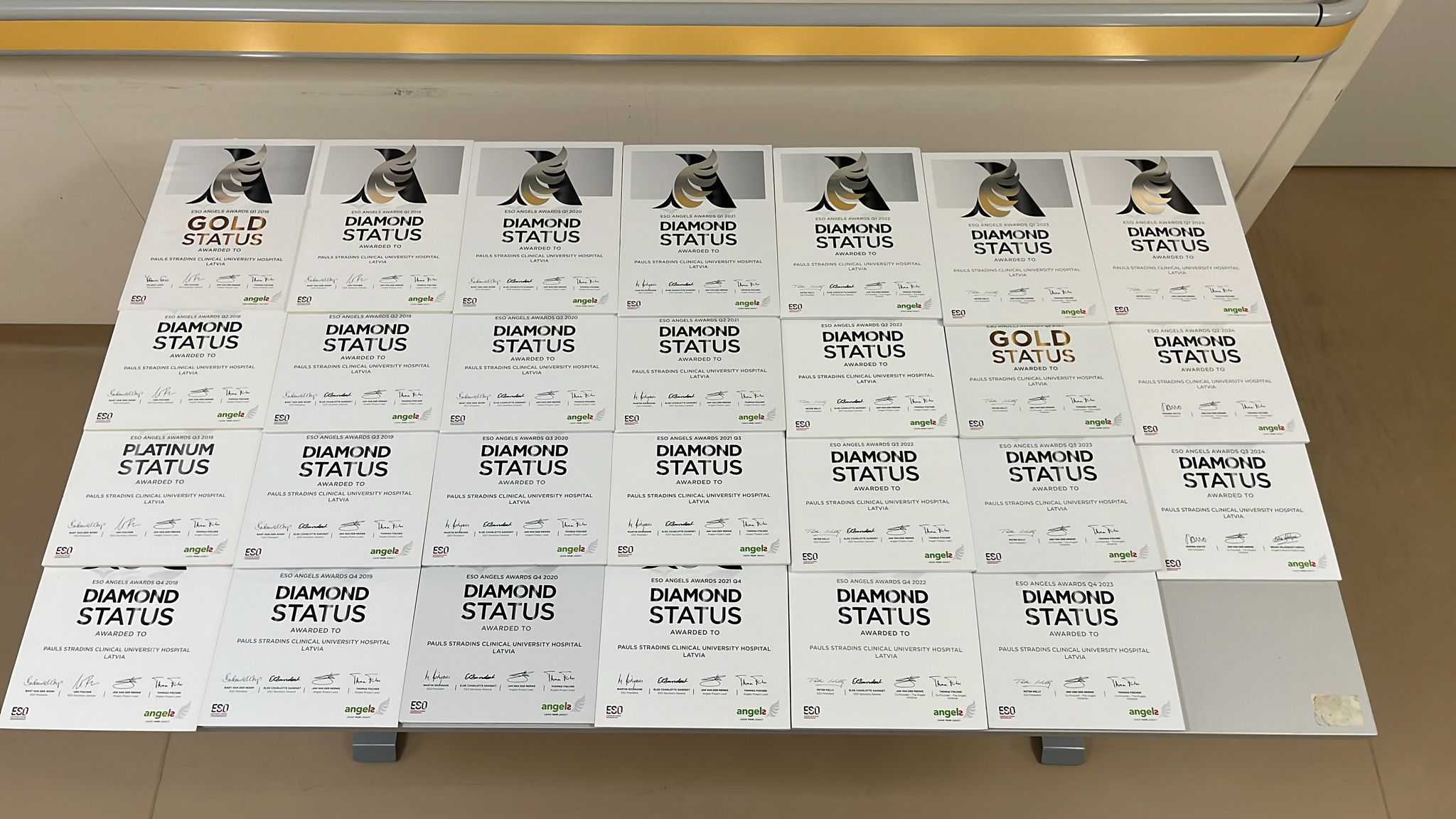
If there was a leaderboard for Angels Awards, Dr Jurjāns’s hospital would be right at the top, with 24 diamond awards and no end in sight. They first put up their hand at the start of 2018 when they registered with Angels, and by the end of that year began a hot streak of diamond awards that would have been uninterrupted but for a missed data entry deadline in the summer of 2023.
“You start something, work at it until you think it works and then you keep doing it,” Dr Jurjāns explains. Once you’ve achieved consistency, treating acute stroke becomes “a routine”, and if it’s a first-class routine then “a second-year resident can make a correct treatment decision in about 10 minutes”.
Dr Jurjāns attributes his confidence to being trained by the most prominent stroke physician in the Latvia and 2020 ESO Spirit of Excellence Award winner, Prof. Evija Miglane. But it was under his leadership that the stroke team at Pauls Stradins arrived on the international stage and has stayed there. During an Angels Train-the-trainer event where he’d been invited as a speaker, Dr Jurjāns joined the audience for a presentation of the post-acute intervention, the Arrow Project, and saw another opportunity to improve.
Developed by three nurses at the Regional University Hospital of Málaga in Spain, the Arrow Project standardizes post-acute stroke care via a system of colour-coded arrows that help doctors, nurses and even porters easily identify the type of stroke and side affected, and via a QR code access details of the treatment protocols for each day, such as regular checks for dysphagia, glycaemia and fever.
Dr Jurjāns was struck by the simplicity and clarity resulting from the use of colours and pictograms including those that indicate whether a patient had been tested for swallowing difficulties and, once tested, what constraints there were on their food intake. Within a few months, an adapted version of the project was taking root in his own stroke unit.

Here was something that might help
Swallowing for human beings is a complex business. It takes around 50 pairs of muscles and several cranial nerves for food to be conveyed safely from your spoon to your stomach – a journey that consists of three phases.
In the oral phase, your tongue collects the food, then works with the jaw to move it around your mouth ready for chewing. Chewing breaks down the food to the right size and texture, aided by saliva which softens the food.
In the pharyngeal phase, the tongue pushes the food to the back of the mouth, triggering a swallowing response that passes the food through the throat. To prevent food or liquid from entering the airway and lungs, the voice box closes tightly and breathing stops. Talking keeps the airways open, which may be why your mother told you not to talk while you’re eating.
The oesophageal phase only lasts about three seconds, during which food or liquid enters the oesophagus, and is carried to the stomach.
It’s a well-coordinated muscle interaction that most people never think about except on those occasions when something they’re eating or drinking “goes down the wrong way”. Then a gag
or cough reflex will usually try to sort out the problem.
If, however, a stroke or other nervous system disorder interferes with the swallowing response, food pieces can block the passage of air, and food or liquid that stays in the airway can enter the lungs, resulting in aspiration pneumonia.
Dr Jurjāns was troubled by a high incidence of aspiration in his stroke unit, affecting up to 30 percent of patients. Here was something that might help. He translated the materials into Latvian and introduced them at his hospital in August, working with a nutritionist and speech therapists to give more substance to the Arrow Project guidelines.
It’s too soon to measure the impact on aspiration rates, but there are clear upsides, including the fact that nurses are now empowered to evaluate a patient’s abilities and they, together with nutritionists, can follow certain pathways for decision making about patient diets rather than only rely on their practical experience.
The pictograms aren’t just helpful to the medical staff; they also help relatives to understand the patients’ nutritional restrictions, Dr Jurjāns says.
One problem he is still trying to solve is variability in the modified textures (categorized as nectar, honey and pudding) that make food safe to swallow for patients depending on their dysphagia score. Here, too, consistency will be the key to success.

‘Make sure he doesn’t get worse’
Dr Jurjāns’s first encounter with a stroke patient was a baptism of fire on the first or second day of his neurology residency. He recalls that the doctor, having started thrombolysis, was called away and left him in charge with instructions to observe the patient and make notes every fifteen minutes. She left him with a terrifying parting shot: “She said make sure nothing gets worse.”
It was an anxious moment for the would-be neurologist who had actually wanted to become an orthopedist. When that program turned out to be full, he surprised his mother by following her footsteps into neurology. They have the same surname and when a patient recently asked her if she was related to “that famous Dr Jurjāns” the first Dr Jurjāne wasn’t altogether pleased, he reports. (She was undoubtedly also proud.)
He became a stroke specialist for the same reason he had wanted to do orthopedics – he wanted to get his hands dirty and in neurology, stroke was where the action was.
“There is always something to fix,” Dr Jurjāns says. Even when you have to keep some of your awards in boxes because the display wall became too small. “It comes in waves for me. Inspiration comes and then I make a change, make something new.”
Some of these changes could appear insignificant – like a pictogram on a clipboard or the Angels Stroke Care at Home manual translated into Latvian to prevent aspiration after discharge – but they do the important work of saving lives.
On the stroke ward at the Regional University Hospital of Málaga where a brief to standardize nursing care developed into the Arrow Project, consistency is also delivering success. They entered the awards table at the end of 2023, and have just won their second consecutive diamond award.
It is reasonable to believe, about any hospital that wins consecutive diamonds, that they have made excellence a habit. Consistency counts. And if you keep doing it for long enough, you will eventually need a bigger wall.



