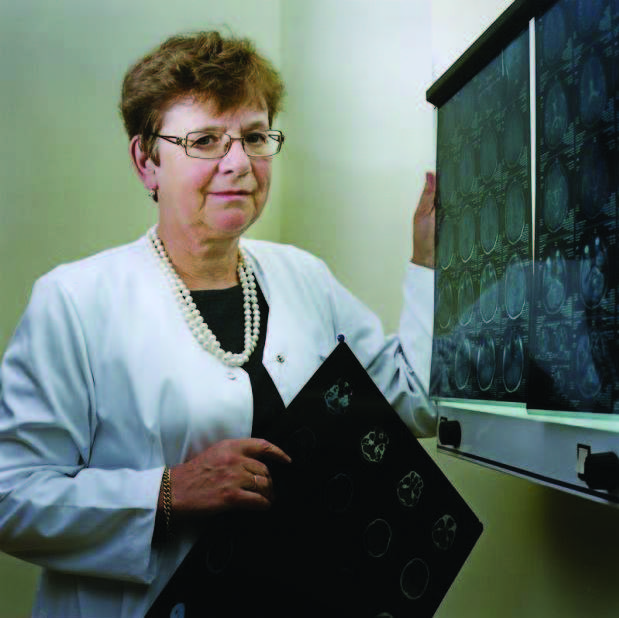
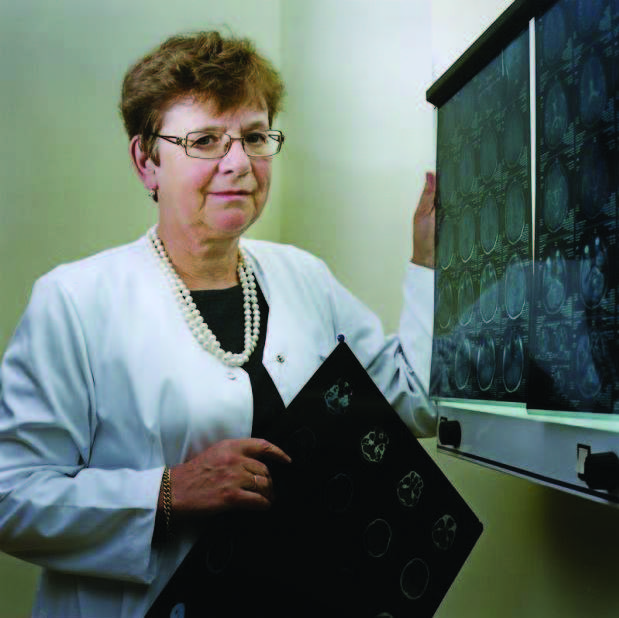
The level of stroke care in Poland has improved greatly in the past years. Under the guidance of people like Prof. Anna Członkowska and others the number of stroke centers grew from just a handful in 2010 to around 170 today.|
Poland did not only focus on more, they also focused on better. In most countries around the world that we have analyzed, we found that they were able to increase the nationwide % of all stroke patients that receive recanalization therapy by on average 1% per year. Poland has averaged around 2% per year from 2010 to 2015! Patient care was transformed, with some reference hospitals now averaging DTN times of 45 minutes.
However, after this initial burst of enthusiastic activity, momentum has slowed down somewhat since 2015 and the numbers seemed to have plateaued to a certain extent. We all know that on a diet, the last couple of kilograms towards your goal weight are always the most difficult to lose and perhaps this is the same for stroke care in Poland.
Should these Polish hospitals that are now already on average DTN times of around 45 minutes consolidate or should they push further to break through the 30 minute barrier like the majority of hospitals in their neighboring country Czech Republic for example?
15 minutes may sound insignificant, but according to a publication by Saver et. Al (2013), every 15 minutes saved in the treatment time of a stroke patient represents an absolute 4% reduction in mortality, 4% reduction in symptomatic ICH and a 4% improved chance of independence at discharge. In other words for a patient 15 minutes may mean the difference between riding a bike or sitting in a wheelchair.
The interesting thing is that we have found while visiting many hospitals across Europe is that there is a very big difference in the mindset for every 15 minutes you add to the DTN time in a hospital. It is as if there are three distinct levels of treatment with three distinct mindsets and varying treatment pathways depending on what level the hospital is targeting.
Observing hospitals that average around 30 minutes or less, you quickly see that they think differently, for them time is an absolute priority. They also act differently by doing a combination of the following things.
- They have a pre-notification system in place with their EMS partners.
- They take the patient directly to the radiology department and don’t waste time by stopping in the ED.
- They interpret the CT on the spot and also treat the patient in the CT room if the patient is a candidate.
- They only consider certain priority lab tests before making a treatment decision and often make use of point of care tests.
Interestingly, hospitals that are averaging around 45 minutes have a slightly different mindset. It’s not that time is not a factor for them as they worked hard to get under 60 minutes, but it’s almost like they are content with the level they have achieved and stopped pushing to improve more. In hospitals like these we often hear concrete reasons why some of the steps mentioned above cannot be done in their unit, or how in their opinion 15 minutes does not make such a big difference.
Hospitals that are averaging around 60 minutes or more often have a very different mindset. In some cases just one or two things that cause major delays like waiting for blood results for example, in others it’s just a general absence of haste. The interesting thing is that those who are now treating patients in 30 minutes look back and say, what did we do for an hour?
In Poland with the personal engagement of Prof. Anna Członkowska and the official endorsement of the National Consultant for Neurology the question now is where to aim for. With significant healthcare and government figures now endorsing the Angels initiative, we are starting to see the momentum shifting again in the right direction.