Hyperacute resources
In the hyperacute phase the focus should be on recanilisation. Every second that the patient’s brain is starved of nutrients and oxygen, the risk of disability and mortality is increased. Any activity that does not relate to recanilisation should not delay treatment in this phase. The same time pressure applies to haemorrhagic strokes.
There are 4 keys that have been shown to reduce the time to recanalisation, these include: pre-notification, taking the patient directly to the CT, treat the patient at the CT, and make use of point of care testing. The tools in this section are aimed at assisting you to achieve this in your hospital.
Checklists
These checklists can be used as an example of how to streamline and standardise treatment processes. Using these checklists will assist in improving treatment consistency during all hours of the day.
-
 REGISTERED NURSE TREATMENT FORM
REGISTERED NURSE TREATMENT FORMChecklists that nurses can make use of which focus on before and during the treatment administration as well as the SNOBS neurological assessment.
-
 EMERGENCY DEPARTMENT PHYSICIAN PACK
EMERGENCY DEPARTMENT PHYSICIAN PACKChecklists that the emergency physicians can make use of which focus on the NIHSS stroke assessment and exclusion criteria for recanilisation treatment.
-
 STROKE PHYSICIAN FORM
STROKE PHYSICIAN FORMChecklists for the stroke physicians to use to assist them in clinical decision making and to gain informed consent for acute treatment where needed.
-
 TREATMENT MEASURES
TREATMENT MEASURESChecklists and guidance on recanilisation treatment, general stroke treatment, brain oedema and elevated intracranial pressure.
-
Personal de TRIAGE prehospitalario- Formulario para el Tratamiento Agudo de pacientes con ACV
Listas de comprobación para el personal de Triage prehospitalario para activación de código ACV inmediato.
-
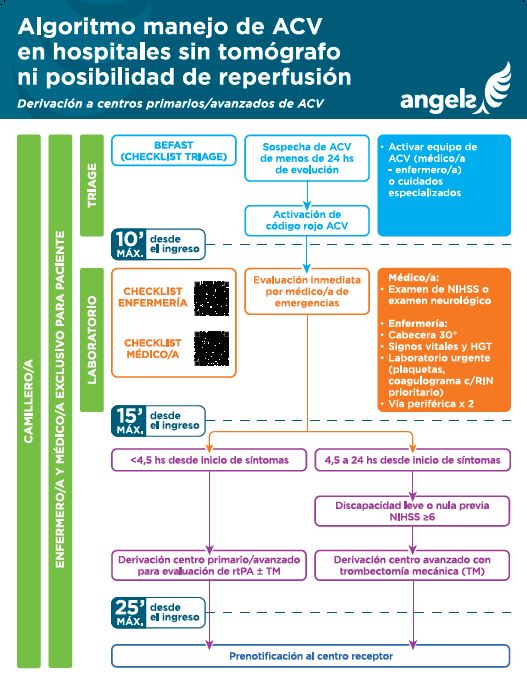
Algoritmo Manejo de ACV en hospitales sin tomógrafo ni posibilidad de reperfusión
Manejo de ACV en hospitales sin tomógrafo ni posibilidad de reperfusión para Derivación a centros primarios/avanzados de ACV
-
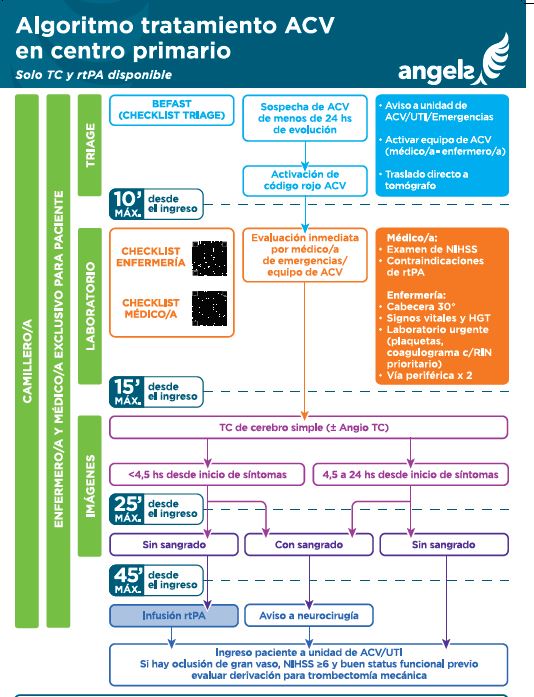
Algoritmo Manejo de ACV en centro primario. Solo TC y rtPA disponible
Algoritmo Manejo ACV en centro primario Solo TC y rtPA disponible .
-
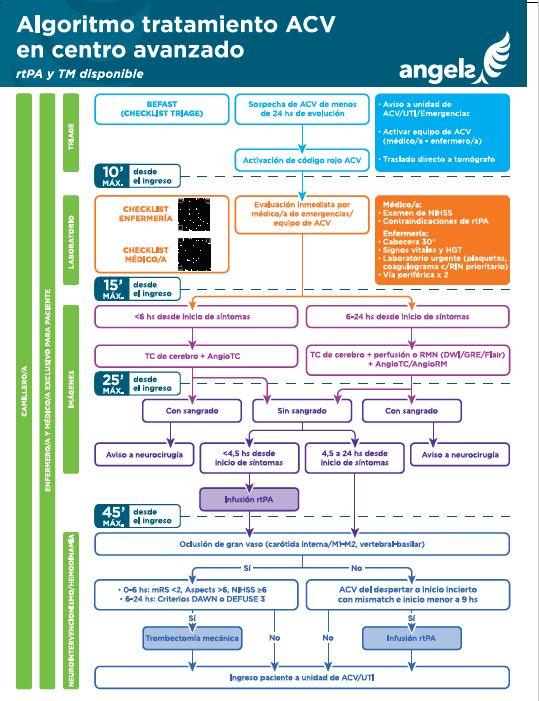
Algoritmo tratamiento ACV en centro avanzado rtPA y TM disponible
Algoritmo tratamiento ACV en centro avanzado rtPA y TM disponible
-
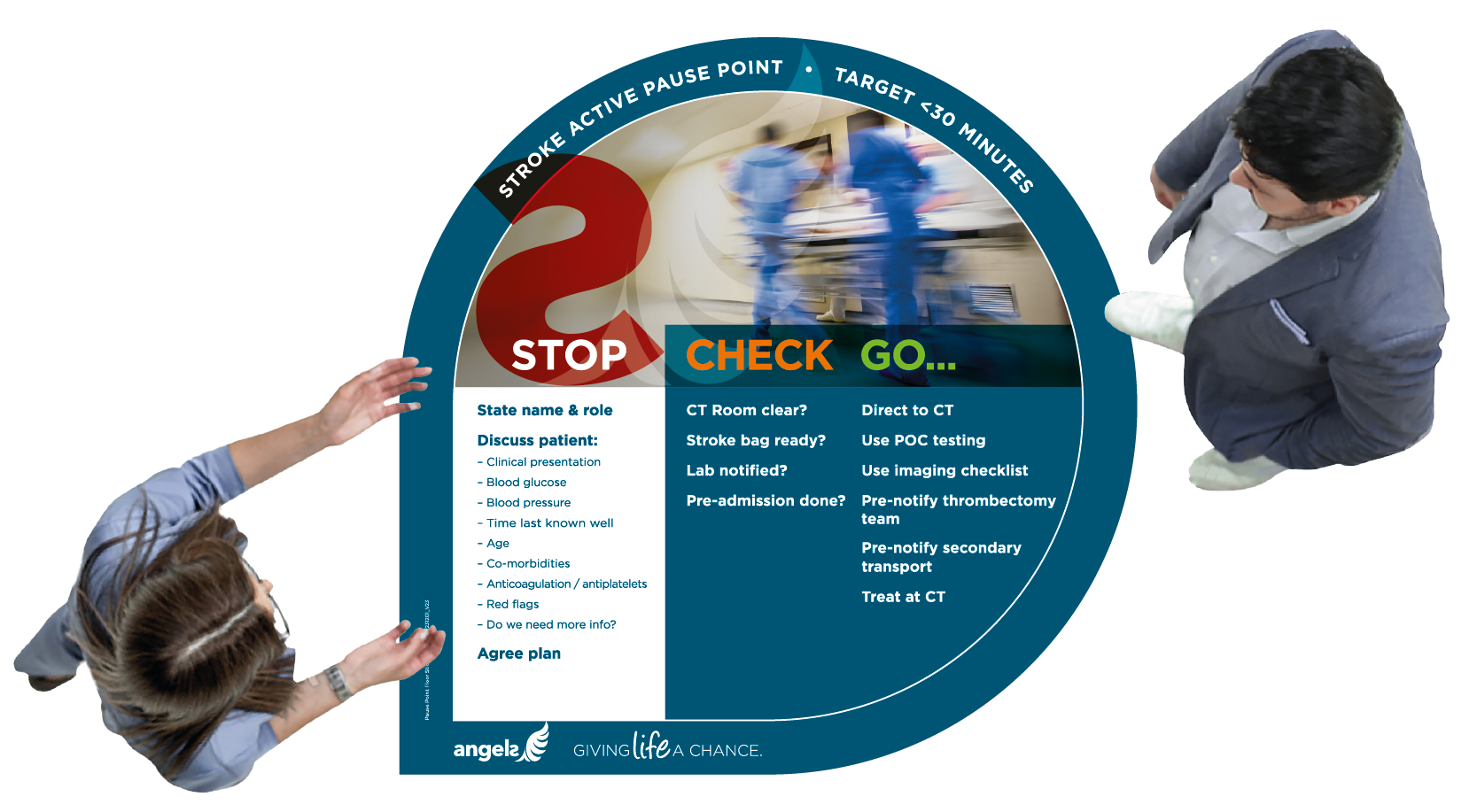 Pause Point Floor Sticker
Pause Point Floor StickerA sticker that will be placed on the floor at key points of hospitals for multidisciplinary teams to share information about the patient and ensure all the correct steps have been taken in the treatment journey.
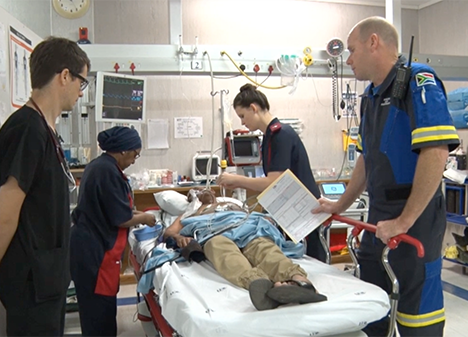
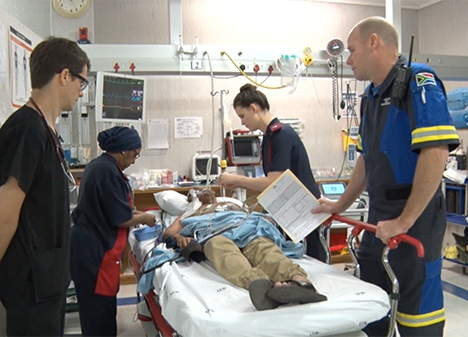
Simulation
Evidence shows that hospitals using simulated patient training also known as dummy patient simulations, have significantly improved their performance in the long-term by improving their door to treatment time.
Simulation training is made up of two parts. Part 1: The stroke team in the hospital assign a simulated patient and is asked to receive and treat the simulated patient as they would for real life stroke patients. Part 2: The hospital should assess the first part and make note of all the improvements and changes that they can make to optimise their pathway and reduce their door to treatment time. Once this assessment has been completed, the hospital should repeat the simulation and implement the changes they have made note of.
Upon completion of Parts 1 & 2, the hospital should assess what improvements can be implemented to the everyday treatment pathway to optimise the quality of stroke care.
Simulation presentation
The simulation presentation serves as guidance for improvement points to optimise the pathway.
SIMULATION PRESENTATION VIDEOS
Download these videos and insert them into the Simulation presentation to enhance discussions.
-
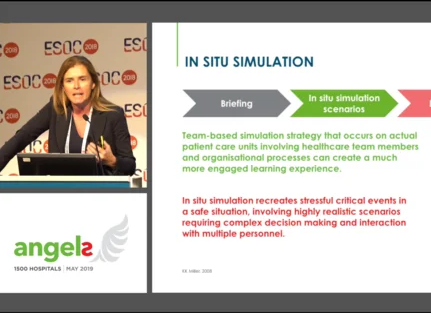 SIMULATION TRAINING TO OPTIMIZE STROKE CARE
SIMULATION TRAINING TO OPTIMIZE STROKE CAREExperience from the ESO simulation committee
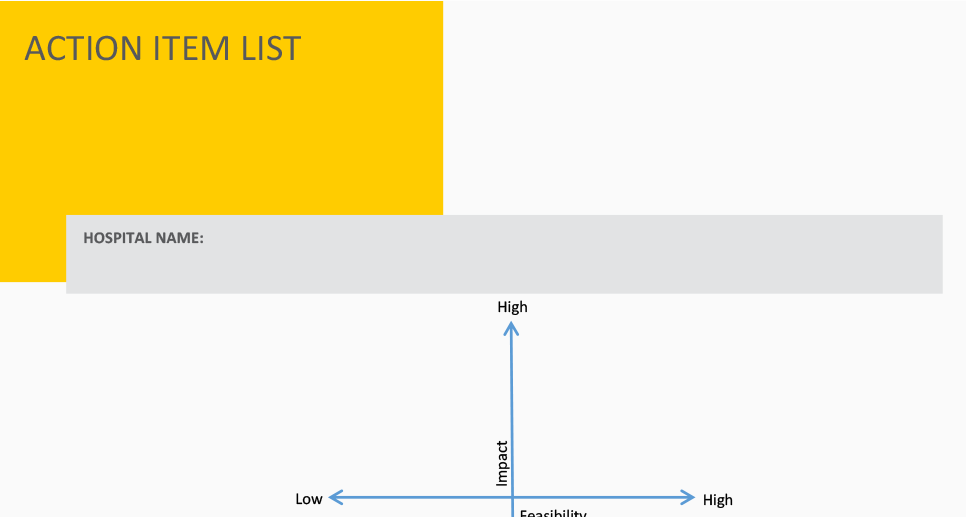
ACTION PLAN DOCUMENTS
Make use of the action plan document to note the improvements and correction actions that can be taken to optimise the pathway to improve the quality of stroke care within your hospital.
PATIENT SIMULATION EXAMPLE
Watch the videos below to see the impact that implementing the 4 key actions could have on reducing door to therapy time.
Resources
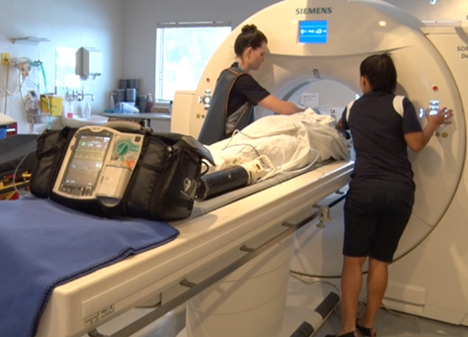
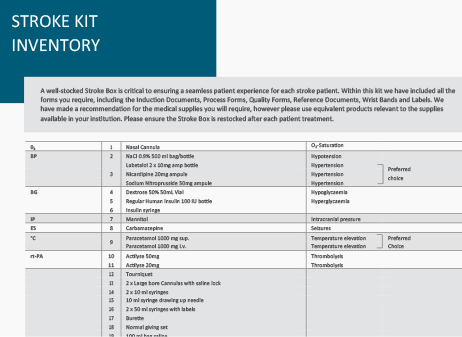
Stroke kit
The stroke kit allows you to carry all the medication, tools and checklists you need with you so that you can treat acute stroke patients in the CT imaging room. Contact your Angels consultant today to find out how to receive your stroke kit.
Take a look at the unique features here
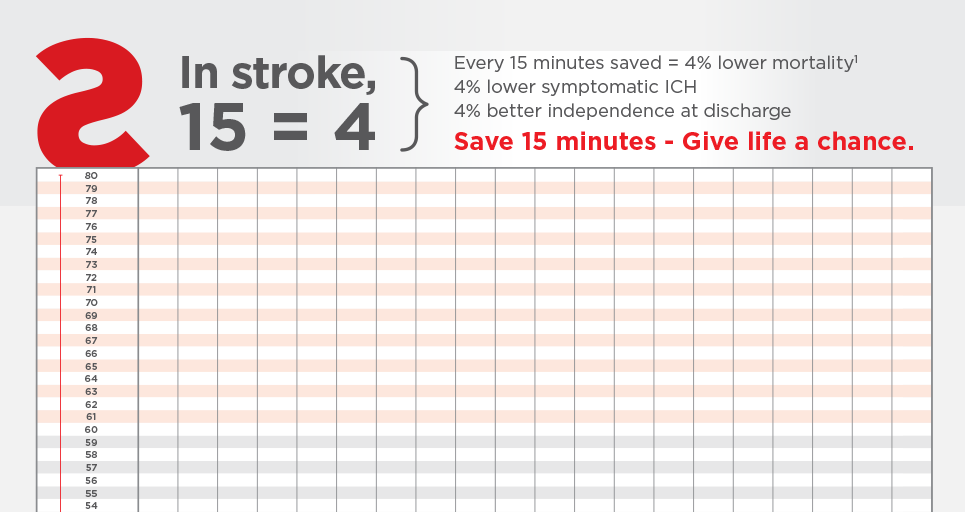
TIME TRACKER POSTER
Log your patient activity to enhance and improve treatment times.
ANGELS STOPWATCH APP
Introducing the Angels Stopwatch App, a simple time-tracker to help stroke care teams build a clear picture of their performance and identify areas for improvement. Additionally, the app has the option for you to share your anonimised data with RES-Q. Download yours today by searching for "Angels Stopwatch" in both the Google Play and Apple app stores.
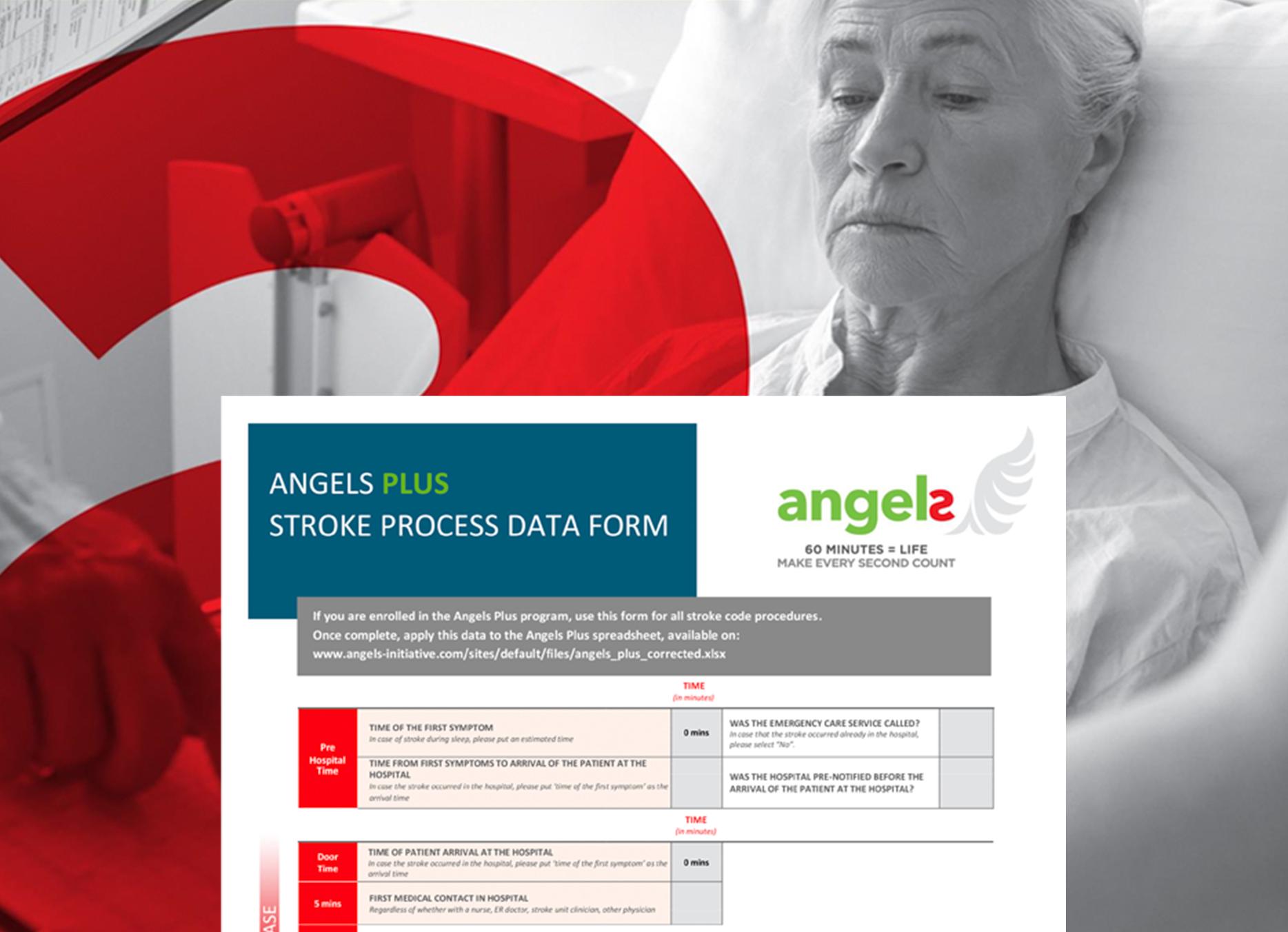
ANGEL PLUS
IMPROVE YOUR DOOR-TO-THERAPY TIME
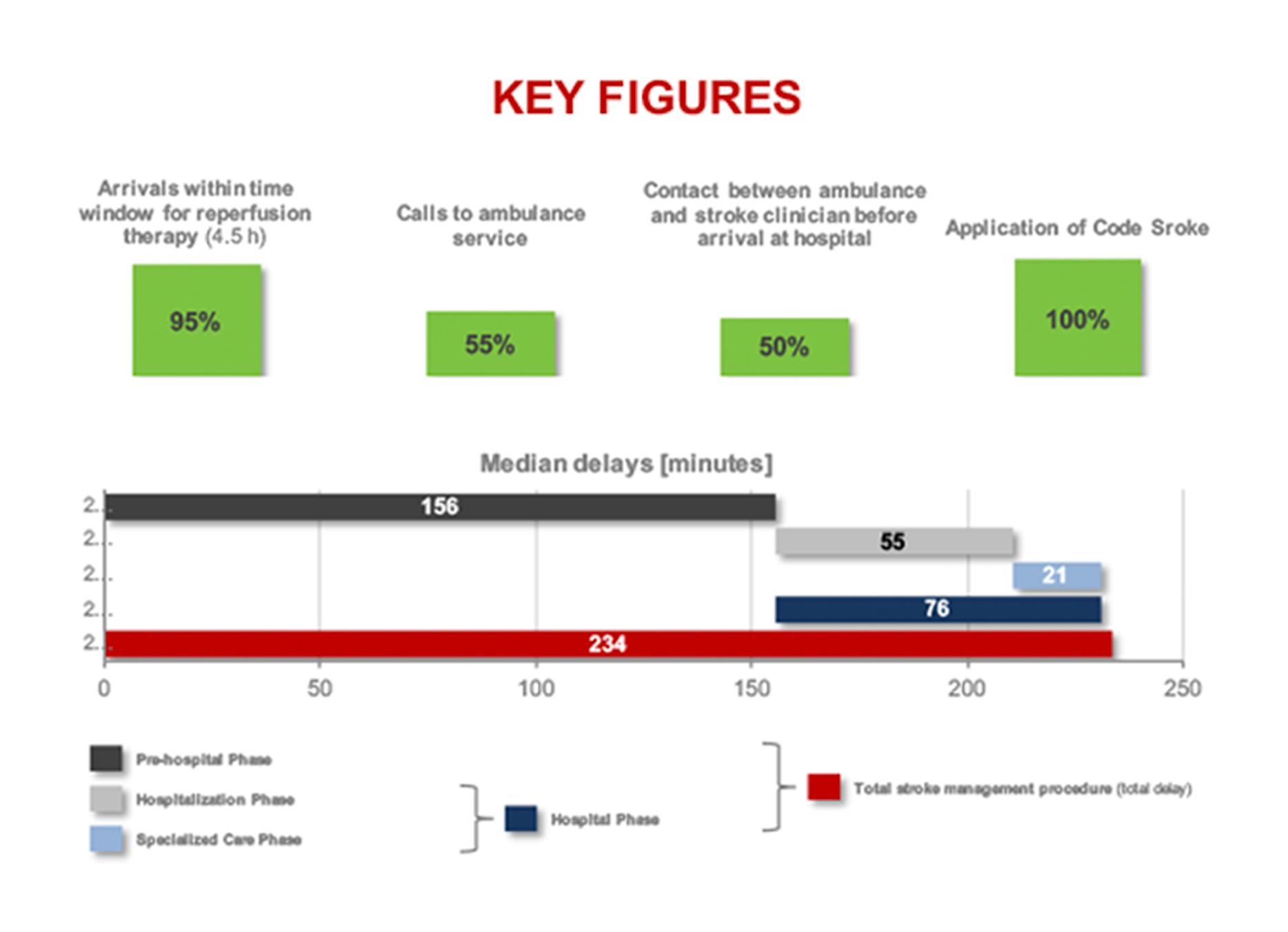
Angels Plus… make every second count. Do you know where you are losing time? Angels Plus allows you to capture the most relevant time stamps and actions. Data is captured and automatically analysed in the Microsoft Excel spreadsheet, stored on your own local computer. It cannot be shared or analysed by other hospitals. Use the Angels Plus PDF and spreadsheet, two useful tools allowing you to capture your data and see where improvements can be made for better patient outcomes.
IN HOSPITAL MOTIVATIONAL TOOLS
The videos and posters below can be used in waiting rooms or hospitals to remind patients and stroke teams of the importance of time.
Workshop Guidance
The hyperacute presentation includes practical tips, workshop ideas, and videos to assisting in improving the hyperacute pathway. The goal of the hyperacute phase is to reduce the door to therapy time to below 30 minutes.
TRAINING THE TEAM
A unique set of assets for you to train your staff featuring the entire patient journey, checklists and procedures.
ADDITIONAL WORKSHOP VIDEOS
These videos can be used as apart of your workshop.
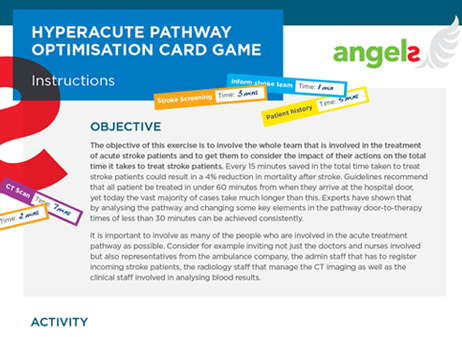
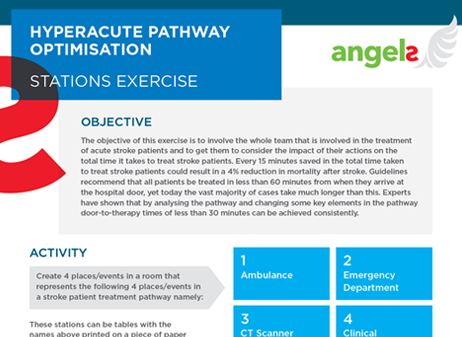
WORKSHOP ACTIVITIES
Practical activities that can be used to challenge the entire stroke care team to consider the impact of their actions on the total time it takes to treat stroke patients. Use these activities to brainstorm and discuss how to optimise your hyperacute pathway in your hospital.