Post Acute Resources
To reduce mortality in stroke the focus in the post acute phase (1-72 hours after treatment) should be on preventing the following most common causes of death: cardiac death (including fatal MI, fatal arrythmia and congestive heart failure), pneumonia, recurrent stroke, sepsis and others.
The goal of the post-acute phase is to improve the quality and consistency of post-stroke interventions and monitoring using the post-stroke and FeSS checklists.
Checklists
-
 DISCHARGE CHECKLIST
DISCHARGE CHECKLISTThe discharge checklist can be used to ensure standardisation of post stroke evaluations as well as ensuring that patient discharge is within guideline recommendations.
Dysphagia training
SWALLOW IN STROKE/TIA
It has been proven that nurse led interventions to manage fever, hyperglycemia and swallow difficulties significantly decreased death and dependency after stroke. Use the following resources to improve and assess your knowledge.
DYSPHAGIA SCREENING & ASSESSMENT PROTOCOLS
Practical guidance for HCPs on feeding tube placement for stroke patients
Stroke Unit
To reduce mortality in stroke the focus in the post acute phase (1-72 hours after treatment) should be on preventing the following most common causes of death: cardiac death (including fatal MI, fatal arrythmia and congestive heart failure), pneumonia, recurrent stroke, sepsis and others.
The goal of the post acute phase is to improve the quality and consistency of post stroke investigations and monitoring using the post stroke and FeSS checklists.
FEVER, SUGAR AND SWALLOW (FESS)
Learn about the importance of performing fever, sugar and swallow screening during the first 72 hours and the best way to apply the FeSS protocol.
stroke care
Find out how to organize the stroke care supply chain and setup a stroke unit
STROKE TEAM MEETING AGENDA
This agenda serves as the basis for the weekly multidisciplinary stroke team meeting that should take place in every hospital. The aim is to briefly present every patient that is being cared for in the hospital at the time of the meeting. Each case should be evaluated from the perspective of protocol deviations, stroke care quality parameters and patient care planning. Following these steps consistently could serve to standardise care and instil a mindset of continuous quality improvement. “To-dos” arising from this meeting can be captured in the Action Items section of this agenda.
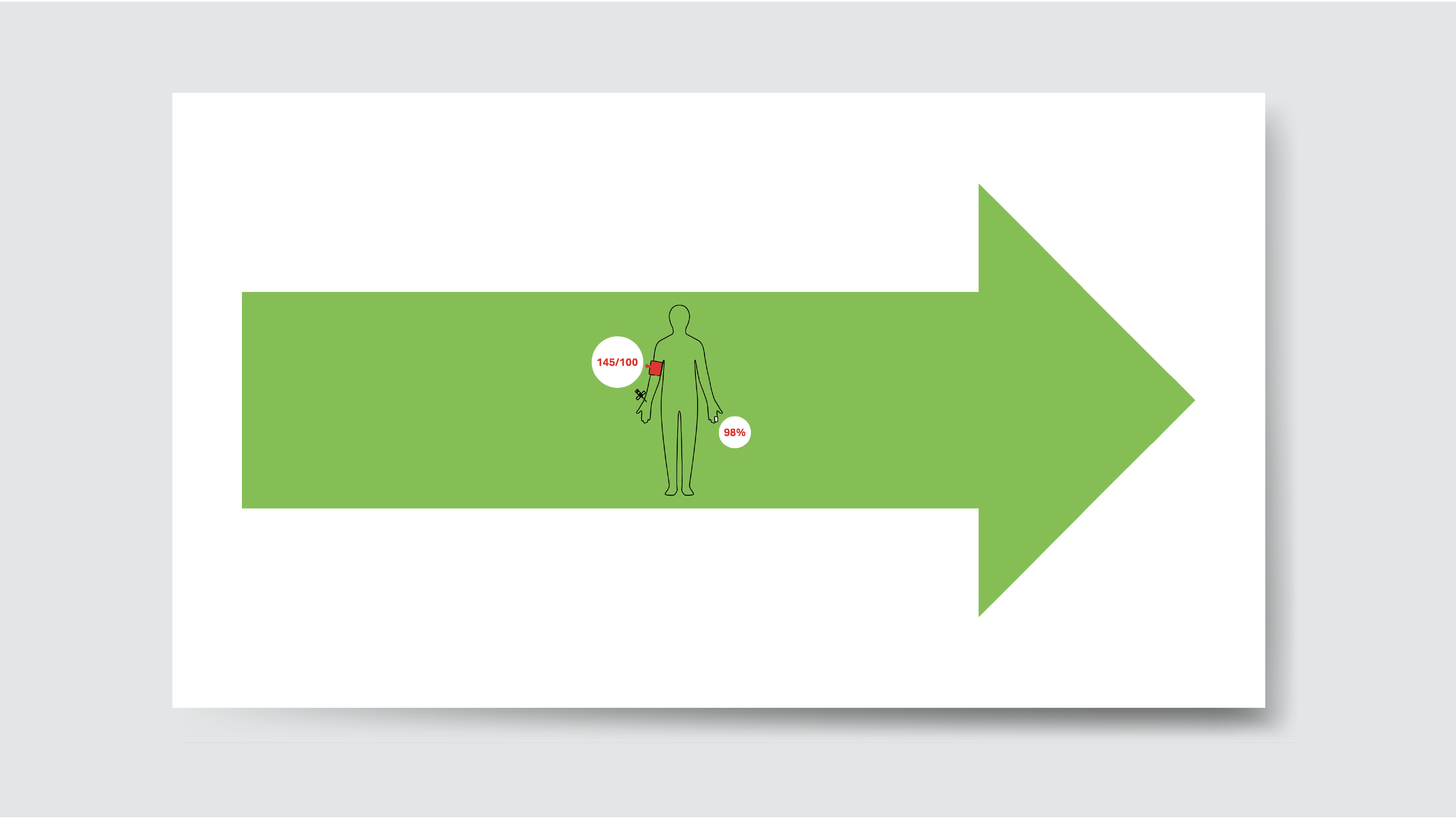
The ARROW PROJECT
The Arrow project standardises post-acute stroke care via a system of colour-coded arrows that are placed above each patient’s bed to help doctors, nurses and even porters to easily identify the type of stroke and side affected. All details of the treatment protocols for each day are communicated via tables – such as regular checks for dysphagia, glycaemia and fever. The first visual cue is the colour of the arrow – red for haemorrhagic stroke, yellow for ischaemic stroke and green for subarachnoid haemorrhage. The second cue is the direction of the arrow. This indicates the affected side so even staff members who have just come on duty will know instantly on which side to place the blood pressure cuff and intravenous line, where to attach the pulse oximeter for measuring blood oxygen levels, how to approach mobilising the patient, and which side is optimal for patients whose communication abilities are impaired.
Resources
-
 STROKE UNIT POSTER
STROKE UNIT POSTERThis poster can be used in the stroke unit as an overview to ensure that key quality indicators in stroke treatment are met.